Breakthrough offers hope for lasting relief from chemo nerve pain
The Challenge of Chemotherapy-Induced Nerve Pain
Chemotherapy has long been a double-edged sword for cancer patients. While it is a life-saving treatment, it often comes with the burden of nerve pain that can persist long after the final infusion. This condition, known as chemotherapy-induced peripheral neuropathy (CIPN), affects up to half of patients treated with certain drugs. Symptoms include burning, tingling, numbness, and electric-shock-like sensations in the hands and feet. For many, this pain does not fade with time, leading to chronic discomfort that can significantly impact daily life.
Why CIPN Is So Difficult to Manage
Clinicians have traditionally had limited options for managing CIPN. Treatments such as dose reductions or symptomatic pain medications often fail to restore normal sensation and come with their own side effects. The condition is particularly associated with platinum drugs, taxanes, and proteasome inhibitors, yet the exact mechanisms by which these agents cause nerve damage have remained unclear. This lack of understanding has made it difficult to develop targeted interventions.
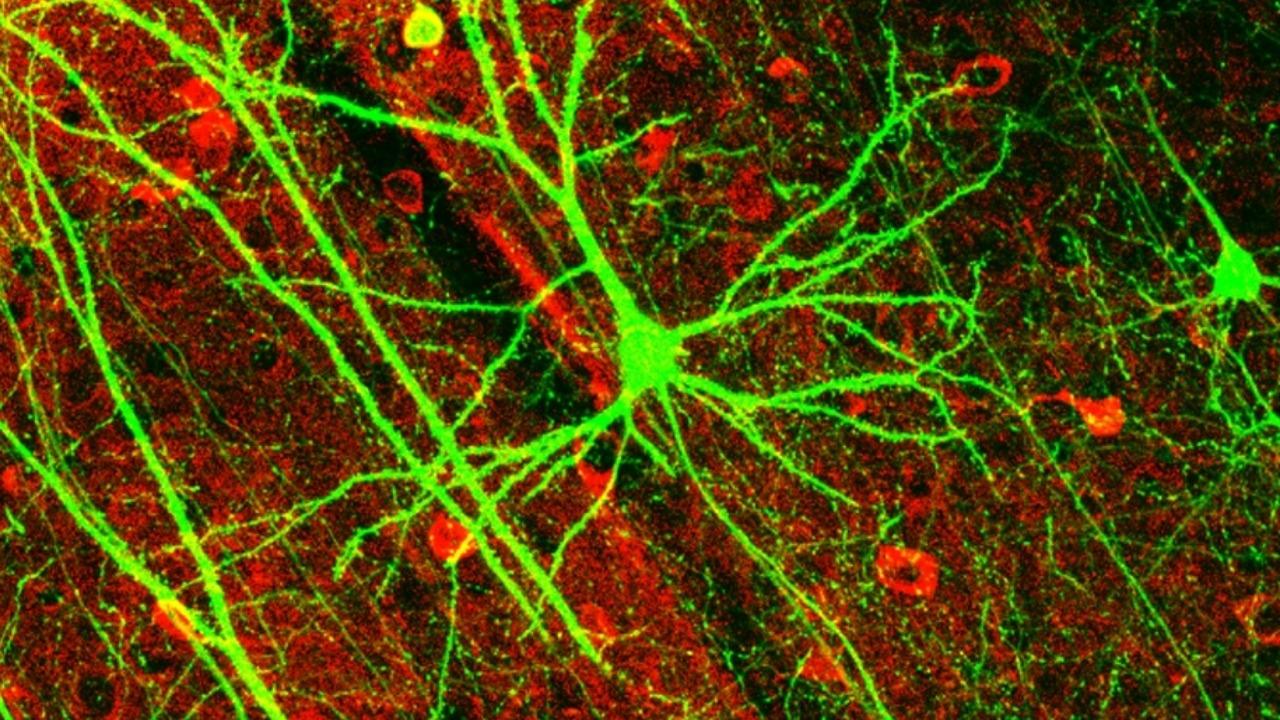
Tracing the Biological Chain Reaction Behind Pain
Recent research has begun to uncover the molecular pathways that lead to CIPN. Scientists have identified a “stress switch” within immune cells that becomes activated during chemotherapy. This switch, centered around a protein called IRE1α, triggers an inflammatory response that damages peripheral nerves. By blocking this pathway, researchers have shown that nerve damage can be reduced without compromising the effectiveness of chemotherapy.
The Immune “Stress Switch” That Could Be Turned Off
The discovery of IRE1α as a key player in CIPN has opened new avenues for treatment. Studies have shown that silencing this stress switch in immune cells can reduce inflammation and protect nerves. This approach not only prevents nerve damage but also preserves the cancer-killing power of chemotherapy. Researchers are now developing drug candidates that target this pathway, with some already entering clinical trials.
Silencing IRE1α and the Promise of Targeted Prevention
In animal models, silencing IRE1α has led to a significant reduction in neuropathic pain. This suggests that targeting this pathway could offer a way to prevent CIPN altogether. Additionally, biomarkers linked to IRE1α may help identify patients at high risk, allowing for more personalized monitoring and treatment strategies.
From Lab Sensors to OSM-0205 in the Clinic
Another promising area of research involves the neuronal calcium sensor-1 (NCS1), a protein that helps nerve cells manage calcium signals. Certain chemotherapy agents disrupt NCS1, leading to toxic calcium overload and nerve degeneration. A drug candidate called OSM-0205, developed based on Yale lab findings, aims to protect NCS1 from this disruption. Early trials have shown encouraging results, paving the way for larger studies.
A “Double Weapon” Strategy to Block Nerve Damage
Researchers at VCU Massey Comprehensive Cancer Center have proposed a dual approach to prevent CIPN. This strategy combines interventions that protect nerves and reduce inflammation, offering a holistic solution that does not compromise the effectiveness of chemotherapy. The goal is to integrate these therapies seamlessly into existing treatment protocols.
Cooling, Compression, and Brain Stimulation: Non-Drug Defenses
Not all solutions involve new drugs. Physical interventions such as cooling and compression of the hands and feet during infusions are being tested to reduce the risk of CIPN. In addition, noninvasive brain stimulation techniques like PEMF are being explored as a way to alleviate symptoms in patients who already have nerve damage.
How New Models Are Reshaping the Science of CIPN
Advancements in research models have allowed scientists to better understand the complex interactions between immune cells and nerves. These models are being used to screen potential drugs, refine dosing strategies, and identify biomarkers that could predict CIPN risk before symptoms appear.
A Crowded Pipeline and What Comes Next for Patients
The growing interest in CIPN research has led to a pipeline of drug candidates from various companies. As these treatments move through clinical trials, they could become standard components of cancer care, much like anti-nausea medications are today.
Why This Moment Feels Different
Unlike previous efforts, current research is focused on specific, druggable mechanisms. The convergence of multiple lines of evidence, including the role of IRE1α and NCS1, suggests that effective treatments for CIPN may soon be available. If these approaches prove successful in larger trials, the trade-off between curing cancer and living with nerve pain may finally be resolved.
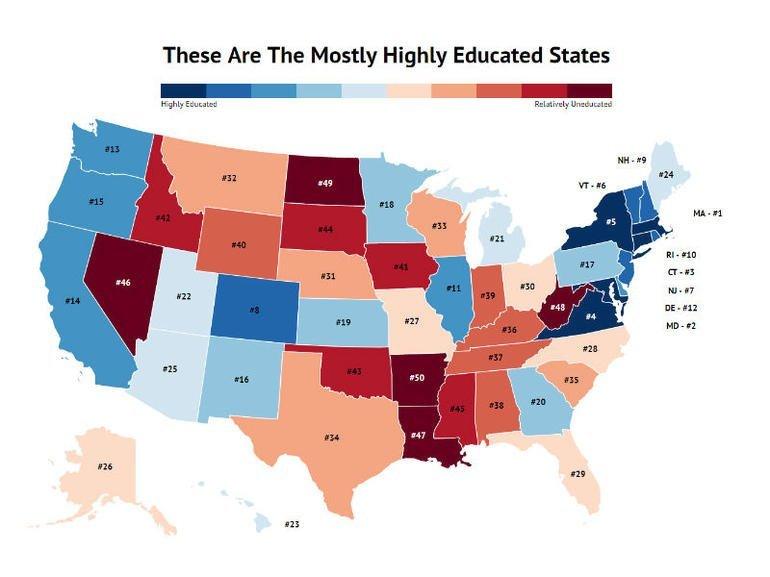
- Top Educated States in America: Is Pennsylvania Among Them? - February 26, 2026
- FDA menyetujui versi generik baru dari obat aborsi kimia mifepristone - February 26, 2026
- Gravitasi Bumi Hilang 12 Agustus 2026, Ini Fakta Sebenarnya - February 26, 2026


Leave a Reply