US strengthens case to maintain measles elimination status amid rising infections
The U.S. Measles Outbreaks and the Challenge of Maintaining Elimination Status
The United States is currently facing a complex situation with ongoing measles outbreaks in South Carolina and other states. Public health officials are working to determine whether these cases are connected to the large outbreak that began in Texas in 2025 or if they represent new, independent incidents. This distinction is crucial for maintaining the country’s status as measles-free, which is a key indicator of public health success.
To be considered free of measles by the World Health Organization (WHO), a country must not have any locally transmitted cases of the same strain for at least 12 months. However, scientists argue that this standard may not be entirely foolproof, especially when it comes to tracking all potential cases linked to previous outbreaks. The challenge lies in ensuring that no cases are missed, particularly in large-scale events where reporting can be incomplete or delayed.
The Texas outbreak, which started in January 2025, spread rapidly and led to additional outbreaks in areas such as the Arizona-Utah border and South Carolina. These ongoing cases continue to pose a threat to public health and raise concerns about the nation’s ability to maintain its elimination status.
In November, the Pan American Health Organization (PAHO), a regional office of the WHO, removed Canada from its list of measles-free countries after a prolonged outbreak. This decision highlights the importance of continuous monitoring and the potential consequences of failing to control the disease.
This year, PAHO will review the U.S. data on measles cases, which include 2,065 confirmed infections. The organization will assess whether the U.S. can retain its measles elimination status, which it has held since 2000. Public health experts emphasize that this status reflects a country’s overall health infrastructure and its ability to prevent vaccine-preventable diseases.
Proving the Outbreaks Are Unrelated
For the U.S. to maintain its elimination status, officials must demonstrate that the current outbreaks are not related to the Texas incident. Instead, they must show that these cases were introduced through infected travelers. William Moss, an epidemiology professor at the Johns Hopkins Bloomberg School of Public Health, explains that traditional methods, such as interviewing patients and comparing viral genotypes, are being used to trace transmission chains.
However, these methods may not always be sufficient, especially in large outbreaks where identifying every case is challenging. Kelly Oakeson, who leads next-generation sequencing at the Utah Public Health Laboratory, notes that many patients did not report travel to Texas or contact with individuals from the state. Despite this, genetic analysis suggests that the Utah strain is distinct enough from the Texas outbreak to indicate they are unrelated.
The Centers for Disease Control and Prevention (CDC) is also using advanced techniques, such as analyzing the entire genetic code of virus samples, to determine if the outbreaks are connected. Early evidence from this analysis, though not yet made public, suggests that the outbreaks are not related. CDC Acting Director Jim O’Neill stated in a December 5 post on X that there is no epidemiological evidence linking the Texas outbreak to the ongoing cases in South Carolina.
A U.S. Health and Human Services spokesman confirmed that the CDC has found no direct link between the outbreaks but noted that many recent cases share the same genotype and have no known source of infection. This could indicate ongoing domestic transmission, complicating the assessment.
Gaps in Data and Challenges in Reporting
Dr. Noel Brewer, an infectious disease doctor at the University of North Carolina, points out that the preliminary evidence suggests the Texas outbreak ended in July, with a three-week gap before the Utah-Arizona outbreak began. No clear connection has been identified between the two events.
Moss from Johns Hopkins adds that gaps in epidemiological knowledge exist, and not all cases are reported. This can lead to missed connections between outbreaks. In addition, some communities with larger outbreaks may not trust the public health system, making them less likely to report cases or participate in investigations.
This lack of participation can result in incorrect conclusions about the relationship between different strains of the virus. Dr. Demetre Daskalakis, former CDC director, acknowledges that PAHO will make its decision based on the evidence it receives. If the organization does not believe in the strength of certain data, it could lead to the conclusion that the U.S. has lost its measles elimination status.
As the situation continues to evolve, public health officials remain vigilant in their efforts to track and contain the outbreaks. The outcome of PAHO’s evaluation will have significant implications for the U.S. public health landscape and its standing in global health initiatives.
- 100 Soal dan Kunci Jawaban Matematika SD Kelas 6 Semester 2 Kurikulum Merdeka 2026 - February 27, 2026
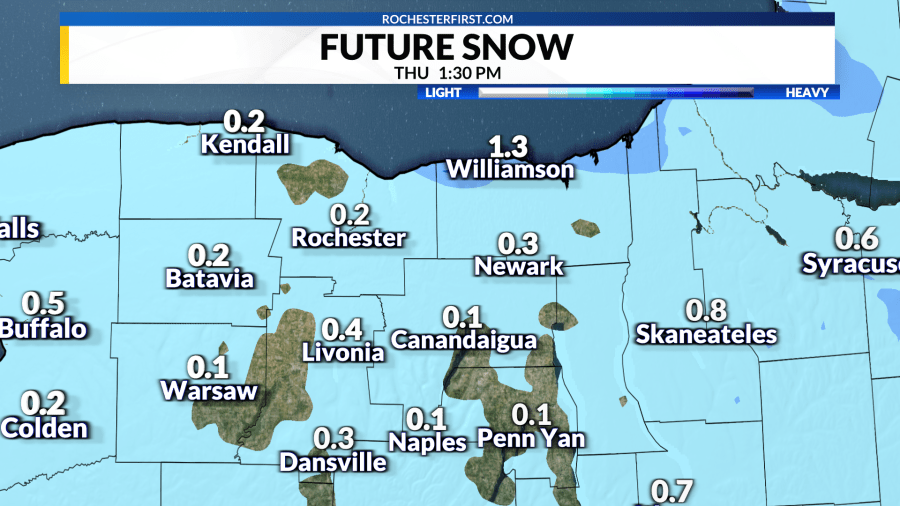
- Light Snow Expected for Lake Areas in the Morning - February 27, 2026
- 50 Keterampilan Dasar yang Harus Orang Tua Ajarkan ke Anak - February 27, 2026


Leave a Reply